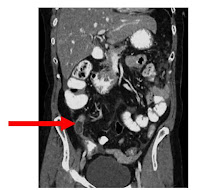
In the year 2000, my aunt and my mother convinced my grandmother to go to the doctor to have a check up. They had been noticing that my grandmother was looking sick and gaining a lot of weight in a short period of time. She only complained of having some minor back pain, but after not going to a doctor for about 30 years, one would start to get used to pain. After being examined by the doctor, she had a CT scan that showed a huge ovarian cyst. The doctor soon scheduled her an appointment with a general surgeon to remove the cyst. They took pictures before and during the surgery. I have uploaded actual pictures of my grandmothers cyst! Recently when I was talking to my grandmother, she said her cyst weighed 29.5 lbs! The doctors that performed the surgery said they had only seen one that was larger, which was 30 lbs.
Ovarian cyst are composed of fluid such as blood, mucous, etc. found inside the ovaries. There are two types of ovarian cysts, one being a follicular cyst, which is basically enlarged follicles, and the other known as a corpus luteum cyst, which is basically a hemorrhage of the corpus luteum (the lining within the ovary). Ovarian cysts are more common in females around childbearing age, but is definitely not uncommon to find them in older women.
Lower pelvic pain, back pain, abnormal bleeding, fullness or a heavy feeling in pelvic area, and painful intercourse are just some of the main symptoms of having ovarian cysts. There can be one or multiple. Misdiagnosis can often occur because doctors mistake it for menstrual cramps. If a cyst ruptures it can cause extreme pain and
Ultrasound is the best diagnostic imaging tool to use, but cysts can also be seen in CT or MRI exams. I have uploaded MRI images. The top image is an example of an ovarian cyst in a T1-weighted image, the bottom is a T2-weighted image (shows a greater signal intensity).
Surgery is done in extreme cases, but the pain can be masked with a narcotic or even ibuprofen. Birth control pills can be given to the patient to help prevent the formation of new cyst.
References:
Eisenberg, Ronald & Johnson, Nancy (2003) Comprehensive Radiographic
http://www.glowm.com
A special thanks is given to my grandmother for letting me use these images.